Getting More For Less
While addressing revenue cycle issues in healthcare varies from region to region around the world due to different payer systems, one thing is for certain –– everyone wants more for less.
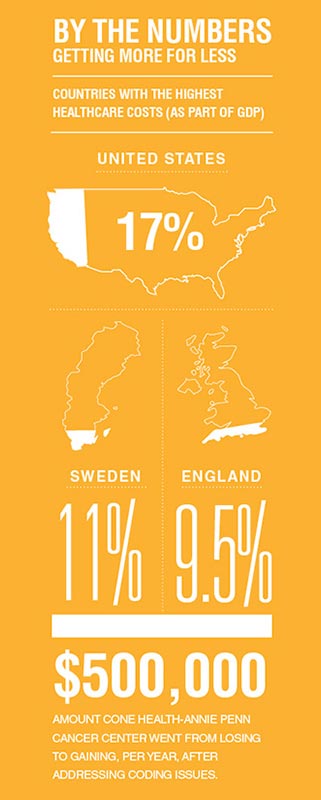
“Fundamentally, the big question is, ‘How do we deliver better healthcare outcomes with less healthcare dollars’,” says Elizabeth H. Bradley, Ph.D., faculty director of the Yale Global Health Institute. (Tweet this!) “The U.S. spends more than 17 percent of the GDP on healthcare costs. This is one and a half times more than any other country. The thing that executives struggle with the most in any geography is how to influence the biggest cost drivers, over which they may have very little control. In particular, healthcare executives worry about how they can impact wellness,” she says.
Dr. Bradley adds, “They can’t control the things that contribute to poor health.”
Jennifer Zimmer, an Insigniam partner, says a large part of the problem is that systems aren’t designed for the future, either for treatment or preventive care. “Today’s systems, especially in the U.S., are based on traditional, fee-for-service financial models,” she says. “They are quickly becoming archaic and need to be redesigned to serve a patient’s goals.”
Corinne Le Goff, president of Roche SAS, agrees, especially as it relates to a growing trend toward innovations in personalized medicine.
“Our system is set up for reimbursement of generalized medicine and is not differentiated for the disease stage,” she says. In oncology, for instance, she says advanced treatments may combine different biologics based on patient’s biomarkers.
“The system is not set up for that,” says Le Goff, who notes that there are reimbursement pilot programs in place, but questions whether actual information technology (IT) systems are up to the task.
“When you talk to the government, it can be overwhelming to say, ‘You have to totally redo your reimbursement system,’” Le Goff says.
The ultimate answer, according to Zimmer, is redesigning the revenue cycle. “While many models are being explored, it essentially involves ‘establishing greater integrity or structural soundness in the way you collect money,’” she says. “The revenue cycle needs to be whole and intact for the realties of healthcare in the future, and, oh, by the way, the future is rapidly becoming now.”
Zimmer cites a recent example with U.S.-based Advanced Homecare (AHC), a very large (Top 75) home care agency, where their process was redesigned to make it easier for patients to interact with the organization, so that multiple financial touch points impact the patient just once.
“When we started in June, Advanced Homecare had significant revenue leakage, losing hundreds of thousands per month on co-pays alone,” Zimmer explains. Today the company is collecting co-pays up front from patients, turning a profit, and, in less than six months, is 80 percent to its fully captured goal.
“The employees, who are on the front line with the patient, now understand the impact their interactions about payment have on the patient experience and on the viability of the company. And AHC is starting to see the money come in. Their approach is the future of healthcare and proof that you can reinvent the process,” Zimmer says.
According to Joel Mills, CEO of AHC, his organization was “stuck,” essentially blaming a new computing system for the organization’s financial issues.
“We were doing enough business to be successful, but not getting the full potential from our hard work,” says Mills. “We were stuck in not being able to bill for all the things we were doing. We weren’t able to focus on the whole business.”
“Reshaping our processes, and putting things in the context of what’s best for the patient, turned things around. It also helped our workforce and leaders to become more engaged,” he adds.
Getting on top of coding issues is another area where gains are to be made, especially in the U.S., where healthcare providers face sweeping changes when new ICD-10 requirements go into effect in October. Mario A. Singleton, MBA/MHA, who is the director of Hematology/ Oncology at Cone Health-Annie Penn Cancer Center, made it his mission to understand and address why revenue wasn’t matching up with volume. Upon doing a deep dive, he discovered that the center was a couple of months behind on billing, largely due to a coding bottleneck.
“I didn’t think we had the proper number of coders to keep up with the volume and after implementing EPIC, our new electronic medical record. After some discussions with our oncology executive leadership team, we brought in contract coders,” he explains. Singleton also did an audit on recent patients and discovered that, in many cases, the system was picking up the wrong J-codes.
“I asked myself if we could get the coding done in five days,” says Singleton. “How would that impact our finances? What if the data was input correctly the first time? ”
When the issues were addressed, the Annie Penn Cancer Center went from losing half a million per year to gaining as much in two years’ time.
“One thing I found was that we needed a strong team lead to oversee the coders and to make them understand their impact on the revenue cycle,” Singleton says. “We needed to paint the picture and let them realize their contributions to the team. We put a strong team lead in place and when the coders discovered that their role was vitally important, they became much more invested in their work.”
Meanwhile, Singleton says his organization is gearing up for the ICD-10 shift, with preparation including training and use of a new electronic records management system that facilitates tracking, both for the organization and patients.
“It is always disheartening and disconcerting when a patient brings in a big binder documenting charges that are incorrect,” he says. “With electronic health records, they can electronically check their bills. It adds a lot of transparency.”
Singleton says he believes that better revenue cycle management is a differentiator and will ultimately help address other strategic issues, including wellness.
“When you are maximizing your revenue cycle management with accuracy, efficiency, and cost-effectiveness, your organization can realize the possibilities of caring for the patients,” says Singleton. “Caring for each other, and the community, while delivering measureable results in areas of quality, service, and cost is something we strive to do daily. Before long, you really can begin to see the possibilities.”



